Another 🇯🇵🇦🇺 talk I gave was on Clinical Informatics/Electronic Health Records (EHRs) in 🇺🇸. How's my definition of clinical informatics?
Making the right information available at the right time to help healthcare teams take care of patients.
Slides/commentary to follow ⬇️
Again — this was only a 30 minute talk, so couldn't go into dramatic depth — just some basic history, pros/cons of our approach, and what I hope for the future.
I grew up in the 80s. (Elder millenial!) How the heck did we get all of our records living in massive paper file rooms in my pediatrician's office to NOW, my patients telling me they don't know their medications because "It's all in the computer?" Let's find out.
One of the most misunderstood (and misspelled) laws of course that started to set things in motion: HIPAA (shoutout @badhippa), which set data transmission and security standards and is where the term "PHI" (Protected Health Information) comes from. It passed in 1996. I was 16.
My *biggest* critique? HIPAA hasn't been updated in 26 years! I first connected to the internet in 1996, and in healthcare we still use FAX MACHINES, mostly because HIPAA said it's okay. (Interestingly I found out Japan still uses fax too—because they have their own HIPAA law.)
8 years later, @ONC_HealthIT is created in 2004 and started the wheels in motion to digitize medical care in the United States. Wikipedia has a pretty decent summary as this slide is a dramatic over-simplification.
en.wikipedia.org/wiki/Office_of_the_National_Coordinator_for_Health_Information_Technology
Probably the next very big piece is the HITECH law passed in 2009. HITECH told hospitals, "Hey we will give you a TON of money to adopt electronic health records, and you can use whatever system you want as long as you meet certain requirements." (TON of money = $$BILLIONS)
HITECH is where "Meaningful Use" comes in, if you've heard that term. A phased approach, baby steps toward a full EHR. It's not that dissimilar from the steps of medical training:
1️⃣Learn to collect data
2️⃣Synthesize/summarize data
3️⃣Make decisions based on data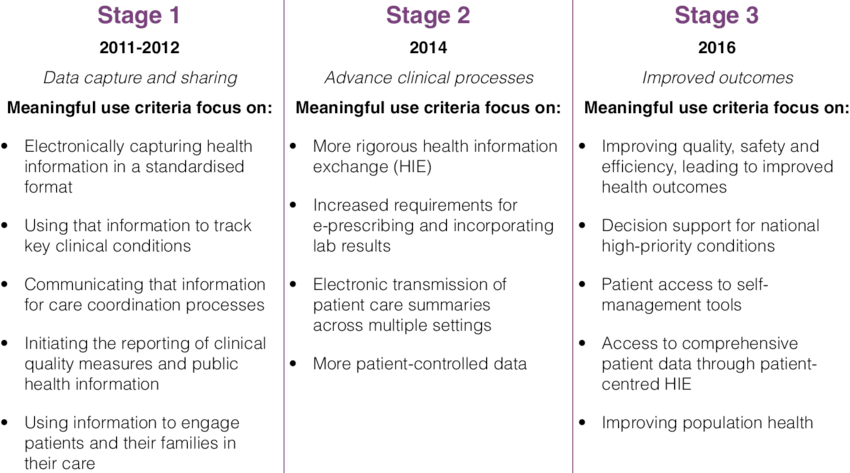
This is how... many things happen in the US. Nothing happens for a long time, and then BOOM💣 a big sweeping law passes to change everything.
Honestly, I'm a little surprised that Congress passed a law with foresight in mind; I can't see our current world thinking 10years ahead.
The "guardrails but otherwise figure it out yourself" approach from Meaningful Use and other policies has lots of pros and cons, like everything in life. Let's cover some.
Flexibility/Choice: Hospitals and private medical practices can choose a system that's best for them. You only do Orthopedics? Great, you can customize your electronic tool to do Ortho and do it well.
But with every new system, you have to re-learn it from scratch.
Incremental Changes: Less disruptive than "Let's change everything all at once," which is probably the right approach in such a critical industry as medicine.
Privacy/Safety: Both are fundamental core principles, baked into the foundation of EHRs. HIPAA specifically called out security standards for storing and accessing patient data, and I'd argue it's pretty clear that computerized orders is safer than paper. psnet.ahrq.gov/perspective/computerized-provider-order-entry-and-patient-safety
We lack a single medical record number for individuals in the US. You can be 100 years old, get all of your medical care for 100 years at the hospital across the street, and my hospital might not be able to talk to yours if you show up my ER. This is extremely wasteful and unsafe
As many informaticists are painfully aware, there is poor interoperability, with lots of data still not available across hospitals/medical systems. Even if I can see the patient's last doctor note, but I can't view their prior CT scan from yesterday or their EKG.
One of the most painful? *Because* it's incremental, healthcare is slow to innovate (or not have permission!)
If I can't get your records electronically? I call the other hospital and ask them to FAX your records to me. If it's night time? You might as well forget about it.
The inevitable dilemma is customization vs standardization. BUT REGARDLESS of how efficient or optimized the system is for one user, generally I think everyone using a standardized place to file data so that everyone can easily access it is way more important for good care.
🔮THE FUTURE: Here's what I'd like to see from EHRs in the next 10 years (curious if people think I'm too optimistic or too pessimistic with my requests)
Make the EHR think more like a doctor. Put CLINICALLY RELEVANT data right in my face!
Patient is there for a head injury? Show me they're on blood thinners!
Recent surgery? Front and center the op note!
They are pregnant? Or have cancer? Make these impossible to ignore!
Auto-suggest stuff to me. Learn from how I've worked in the past.
"Dr. Walker, I see you tend to order these tests when a patient over 65 presents with HIP INJURY. I've already ordered them for you, please review them and click sign."
Doctors spend SO much time writing notes and documenting. I absolutely love this demo from @GoogleHealth showing that as you type, the system provides you context-relevant information and helps you write your note and make it relevant and worth reading.
youtube.com/watch?v=P3SYqcPXqNk
Automation: I love this idea of using AI/deep-learning in less-resourced countries to help find tuberculosis on chest x-rays. Brilliant work.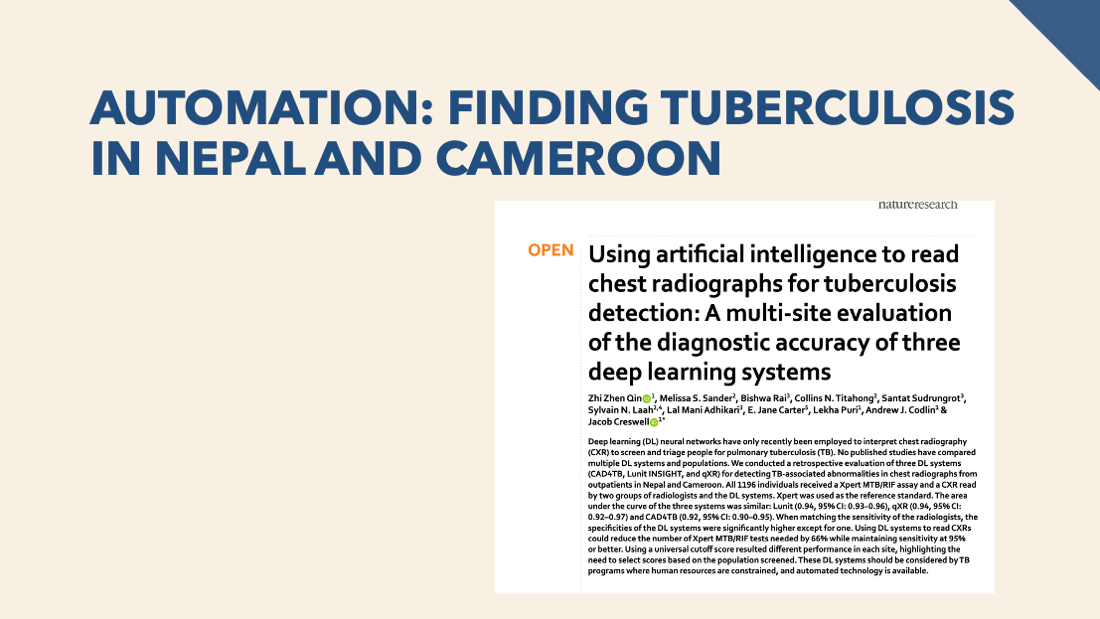
Prioritization: Machines are better at doing tasks in parallel. Radiologists can read an XR better than a machine, but machines can analyze 1000 XRs at a time.
Here AI re-sorts XR reading queues so a radiologist can confirm abnormals and make diagnoses faster.
Prediction: Please, let's make our prediction/risk tools *more* complex, not less! There is no need to make scores +1 +2 +3 points; let a computer do the calculation and give more accurate results! cc @mdcalc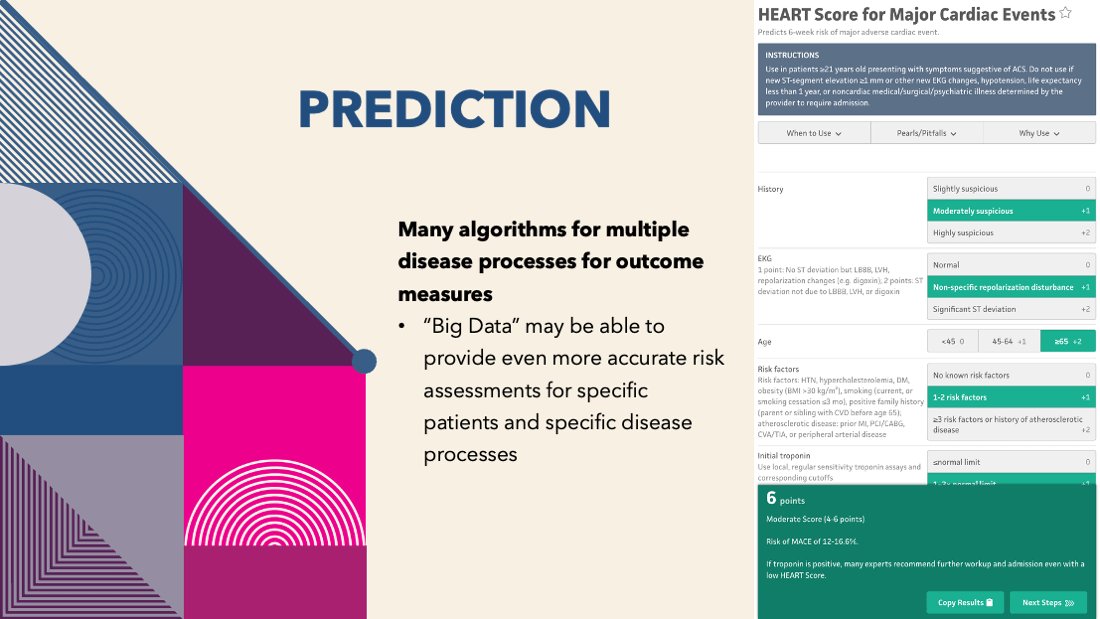
Many physicians use scribes (people that follow them around and document for them) to save time and money on writing notes. The future version of this? Live transcription, where a machine listens to questions and answers and documents for you in real-time, just like a scribe.
Live Translation! Please! In my ER there are at *least* 6 languages spoken every day, and probably more like 15/week with our patients. Powerpoint will actually already live translate a presentation for you. I need this in my ER!
support.microsoft.com/en-us/topic/using-microsoft-translator-in-a-presentation-2582d976-97ea-4bf3-af1b-3647d925240a @Health_IT @drhew
And finally, I included what Twitter thought I should talk about in Tokyo and Sydney, via this thread:
twitter.com/grahamwalker/status/1531723122943983617?s=20&t=5oE_RnCqm7xDO9QGsk3Leg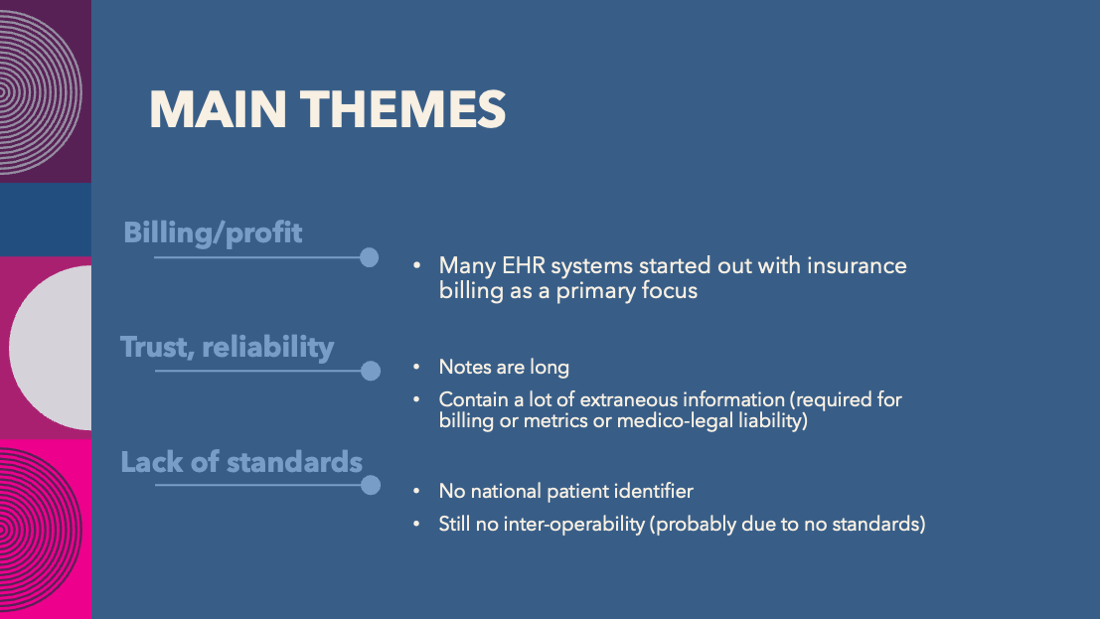
My favorite pieces here are from @nickgenes showing how ridiculously long American notes are...
twitter.com/nickgenes/status/1531786979209355264?s=20&t=5oE_RnCqm7xDO9QGsk3Leg
And @subhaairan showing that 6 years of charts is 8x longer tham all of English Wikipedia! twitter.com/subhaairan/status/1536858397332672512?s=20&t=5oE_RnCqm7xDO9QGsk3Leg
Finally, luckily we have a little bit of movement on a national patient identifier...
Tag your favorite informaticist to contribute!
@MattSakumoto @dirkstanley @cddirks @bspartridgeCIS @psevillemd @Lee_MD_IT @nickgenes @mpvancuyk @danmunro @jayparkinson @davidrosenthal @mshlcurrie