New emergency medicine level of service billing changes coming in 2023! @EmergencyDocs @ACEPNow @JeffreyLDavis44 just released a really helpful FAQ, thread calling out the big points: 🧵
FAQ here acep.org/administration/reimbursement/reimbursement-faqs/2023-ed-em-guidelines-faqs/
In case you missed the prior thread with an overview of the changes, thanks again to @RobPNorris. Now on with the FAQ:
twitter.com/grahamwalker/status/1573430425069887489
No, you don't have to include all the long ROS, PE, Social Hx, etc. BUT your H&P should include pertinent info to tell the story/support your MDM (and don't forget medico-legal stuff).
Ex: If you're gonna "count" MDM points for "independent historian" you better mention who&why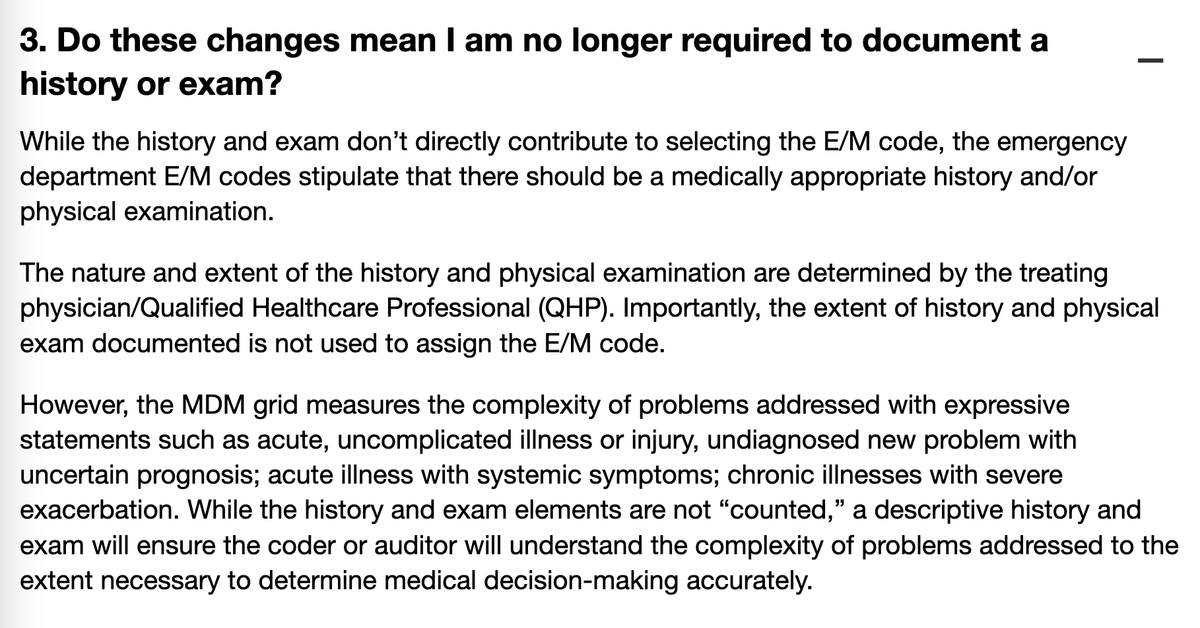
An ER-focused table/grid is available here as a PDF: dropbox.com/s/pg1xt9hnk97zjnz/ACEP%20-%202023%20ED%20MDM%20Grid.pdf?dl=0
As a reminder your "two highest MDM categories" yields the final CPT code 99282-99285 (bye 99281! 👋)
The PDF lays out the columns much better, gives examples pertinent to EM. Bravo. 👏
Number & Complexity of Problems Addressed (COPA): Very nice list of examples of what "minor&major" and "stable & complicated" can mean.
It's a little overwhelming but I think we'll get used to it with time. Roughly:
Admitting = High
Working up = High/mod
Rapid Care = low/mod
Again, roughly:
Amount and/or Complexity of Data just kind of sucks. It's awkward, you have to count points of sub-categories, etc. It's really worth reading the FAQ but I'll go into the important subtleties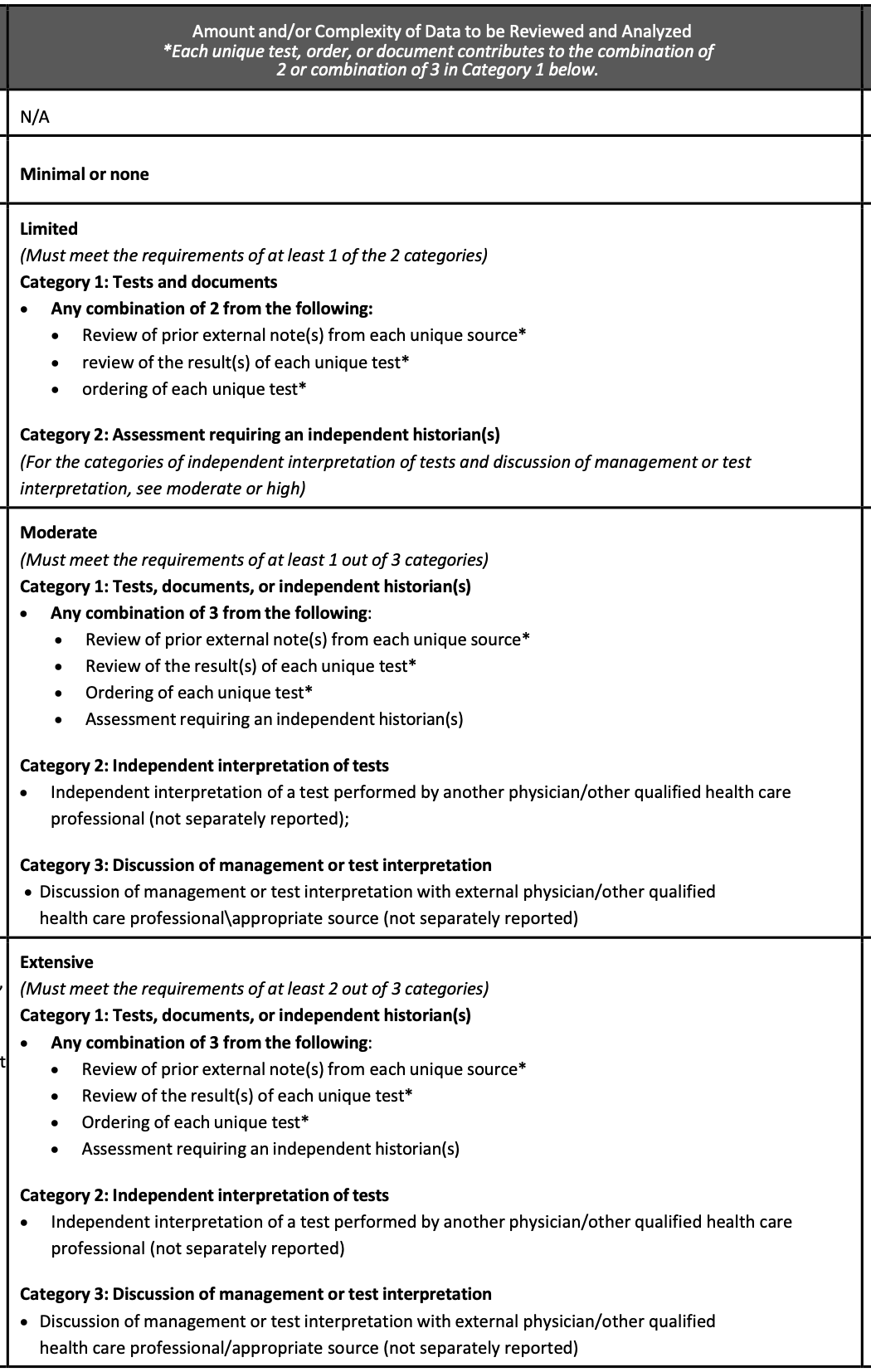
VERY IMPORTANT:
ALL CATEGORY 1 POINTS CAN JUST COME FROM ORDERING TESTS, which is probably going to be the easiest way to document satisfying these criteria (since if you're working up a patient, they're getting several tests like CBC, Chem7, UA, etc)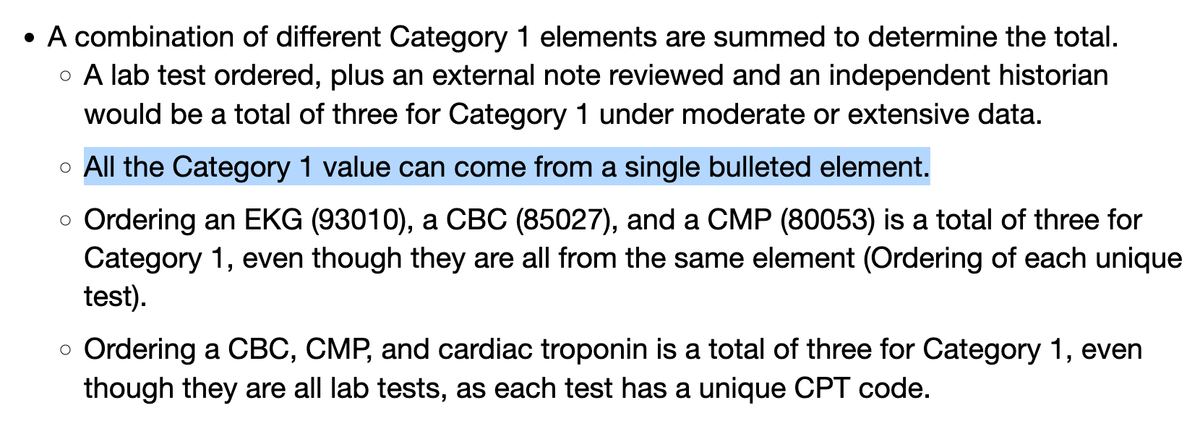
Interpreting labs — "high BUN/Cr ratio, anemia, will do rectal exam for syncope" does NOT count for "independent interpretation," only things like you giving your read of an EKG, XR, rhythm strip, etc.
For category 1, "external notes" is literally anything outside of the ED — could be a clinic note, inpatient chart, nursing home note, even an EMS report.
The only time you're not gonna get a point for this is if the patient walked in and they're literally a blank slate.
So I think generally patients getting any workup more than Rapid Care — will be "moderate." Maybe "dysuria" you're ordering a test but treating empirically, so they would be "limited," but even most ankle sprains will get 1) XR 2) XR interp by you 3) review of their prior records
Independent historian (Category 2) is literally anyone that's not the patient, (including parents of children), MINUS interpreters of course
Discussion of management (Cat 3) is any consult — could even be staff of a nursing home, home health, etc (ie: not necessarily a doctor)
BUT you must do the discussion, not a nurse or case worker
The last column - amount of risk or morbidity/complications is probably super intuitive since most of our job is risk stratification.
Will this take a bit of time to get used to, especially the "Amount/Complexity of Data" rules? Yeah. But I think probably within 6 weeks we'll all have a general sense of where patients fall based on their chief complaint, co-morbidities, workup needed, etc.
General rule is if you're gonna "count" something toward MDM, it needs to be documented. (Something you probably already do more or less.)
But I think if you're giving IV morphine, that's already in the MAR and you probably don't need to call it out in your note?
I think overall it's a major major improvement, and over time will hopefully reduce note bloat, clicks, and garbage in clinician notes. Like everything in medicine, it was only about a decade overdue for change. Thanks again for the FAQ via ACEP and the Documentation/Coding team!