Some of the most challenging cases on the leukemia service were patients who seemed totally stable but wouldn't stop fevering!
#OncID is one of my favorite parts of cancer care.
Let's talk inpatient neutropenic fever!
- Thread -
#MedTwitter #MedED #FOAMed #OncTwitter
Check out the neutropenic fever inpatient template @pointofcaremed
pointofcaremedicine.com/hematology-and-oncology/neutropenic-fever
Also, check out the podcast and a video with accompanying slides on our new YouTube channel!
spotifyanchor-web.app.link/e/lGRz5aFLNwb
youtu.be/PwrwWZIe6ik
Interestingly, there are many different definitions of fever depending on the context.
A fever is technically any temperature above "normal."
The Merck Manual defines fever as an oral temp >37.8 C (>100.0 F) OR a rectal temp >38.2 C (>100.8 F)
Neutropenic fever is a unique subset and is defined as a T >100.4 F with an ANC <500, or an expectation that the ANC will be <500 within 48 hours.
Most patients fully recover without complications, but some go on to develop severe sepsis.
As such, any patient who meets these criteria should receive antibiotics.
The decision to treat inpatient or outpatient is mostly based on the clinical context.
Many patients will have risk factors prompting admission for IV abx.
The MASCC Risk Index Score can be helpful for identifying low-risk patients who can be treated outpatient, but it includes subjective criteria.
In general, patients are at greater risk if:
- SBP < 90
- Heme malignancy w/ prior fungal infx
- > 60 yo
- h/o COPD
When admitting a patient, helpful information to find in the chart includes:
- cancer type
- last treatment and date
- last known WBC and ANC
- prev micro data (look for MDROs)
- recent abx use (including ppx)
- recent healthcare exposures
- indwelling lines
When seeing the patient, ask about:
- timing of fevers
- subj vs obj and Tmax
- sick contacts
- localizing sxs
- travel
- exposures
Check out this @pointofcaremed template for a full ID social hx, and look out for a future thread on this topic!
pointofcaremedicine.com/infectious-disease/id-social-history
Initial workup:
- CBC with diff
- BCx at 2+ sites (always include central line if there is one)
- UA/UCx
- CXR
- lactate
Add RVP, procalcitonin and consider CT chest if c/f pulm source
Add stool cultures, O+P, CDiff if diarrhea
Consider BDG and LDH if RFs for fungal
An infectious source is identified in only ~30-50% of cases. Of these, ~60% are GPCs and ~40% are GNRs.
Despite this, the focus of antibiotic selection is on covering for GNR bacteremia, as this can lead to rapid deterioration 2/2 sepsis.
The source of GNR bacteremia is most likely from translocation of enteric bacteria.
This is one of the main reasons we forgo DREs in patients with neutropenia.
Abx choice is based on both guidelines and local antibiograms.
Most inpatients initially receive cefepime or zosyn monotherapy.
Vanc can be added for GPC/MRSA coverage if pt has severe sepsis, c/f catheter-associated bloodstream infection (CABSI), or severe mucositis.
The decision to add fungal coverage is tricky.
A positive 1,3-BDG can be helpful.
It tests for a cell wall polysaccharide unique to fungi.
It has good sensitivity but is not specific and is seen in PJP, aspergillus, candida, cryptococcus, and rhizopus.
However, you may have to make the decision without fungal labwork results.
In general, it makes sense to consider fungal coverage if the patient has any of:
- severe sepsis
- CT with GGOs and/or nodules
- fevers for 4-7 days despite BSAs
- prolonged ANC <500
- TPN use
Voriconazole and posaconazole are preferred for empiric coverage because they also cover aspergillus and endemic mycoses.
Fluconazole should be used when there is a confirmed candidal infection.
@MatthewHoMD tweeted out a much more detailed flowchart for making treatment decisions for neutropenic fever. @ambossmed
Definitely check it out:
twitter.com/MatthewHoMD/status/1478937599049977864
Looking forward to consulting him next year!
Despite BSA, patients can continue to have fevers.
A schema for approaching such patients:
- wrong bug (viral, fungal, atypical)
- wrong drug (MDRO)
- wrong process (not infection)
- No source control
- Not enough time
Look out for a future thread focused on this topic!
A common cause of ongoing neutropenic fevers is a lack of source control.
The decision to pull an indwelling line is based on blood cultures not clearing or the growth of staph aureus, pseudomonas, or fungi at any time.
CT C/A/P can also help identify a source.
So when do we stop abx?
If you have positive cultures, narrow based on susceptibilities and treat per usual based on the infection.
Otherwise, continue empiric BSAs until there are no fevers for ~4 days.
Then treat with a PO fluoroquinolone as ppx until ANC >500.
If you remember nothing else:
- Most patients never have an identifiable source of fever!
- Treatment is based on empirically covering for GNR bacteremia
- Adding gram pos or fungal coverage is based on clinical status and RFs
- If pt is stable, is okay not to broaden!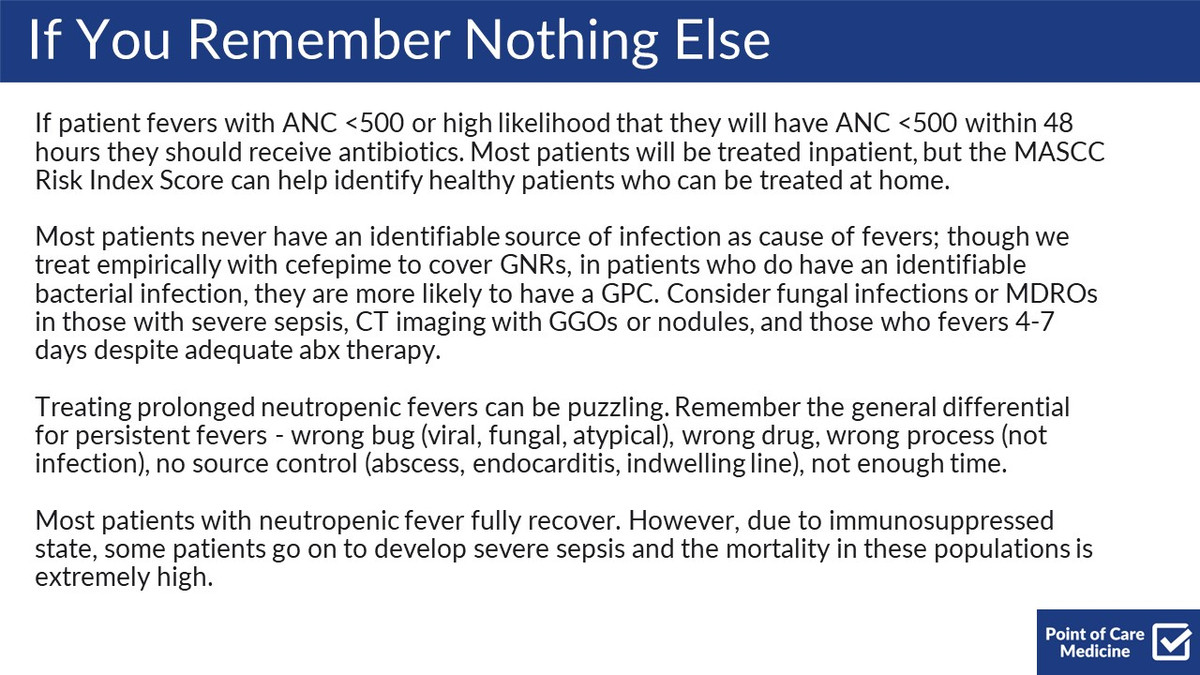
Other great resources:
@thecurbsiders Podcast #288
twitter.com/thecurbsiders/status/1422169793910747138
@OsmosisMed Review article
osmosis.org/answers/neutropenic-fever
An excellent review in JCO:
Optimal Management of Neutropenic Fever by Dr. @AndreaJZimmer and Dr. Alison Freifeld
ascopubs.org/doi/full/10.1200/JOP.18.00269
@MatthewHoMD
@AndreaJZimmer
@TimothyJBrownMD
@lukasronnerMD
@ASanchez_PS
Calling on the experts and colleagues!
Anything you'd want to add or clarify?
Do you have any favorite pearls for neutropenic fever management?